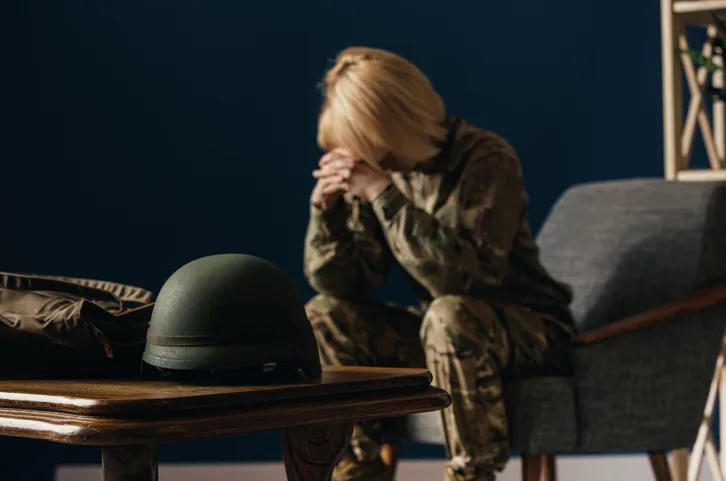
Katie* joined the Marine Corps in peak physical condition. As a Division 1 college athlete who rowed crew, she breezed through military officer training and passed physical testing with flying colors. However, 10 years into her military career her first pregnancy caused pelvic floor damage that never fully recovered despite efforts to return to physical training and meet weight standards for rejoining six months post childbirth – creating additional stress on her body that forced chronic back and hip pain which limited physical activities while necessitating medical providers for pain management services.
Katie described how pain can build up over time without ever receiving adequate treatment, leading to “an endless cycle wherein your nerves seem stuck in an inexorable spiral,” leading her into believing the discomfort would go away on its own. “Because pain was left untreated for so long, the problem continued unchecked.
While approximately 30-30% of female military veterans report chronic pelvic pain – at double the overall rate among civilian women of childbearing age – Shea O’Neill, M.D., an OB-GYN specialist working at Naval Medical Center San Diego noted there was no one aspect of combat deployment or military training that directly caused such symptoms; rather it can trigger stress and trauma which lead to physical responses from their bodies.
Watch: Reducing Pelvic Pain in Servicewomen
O’Neill acknowledged the difficulty associated with deployments and war, noting any kind of trauma will likely affect one’s menstrual health in some way.
O’Neill sees nearly all servicewomen and service members assigned female at birth (AFAB) seeking treatment at the medical center who report pelvic pain. Her work as a detective necessitates questioning patients about their histories to locate sources of discomfort; to do this she must question recent trauma as well as past unresolved events that might prevent healing and recovery; such conversations may begin by discussing recent trauma such as sexual assault but then reveal deeper issues, like grief over parental death in childhood that can contribute to physical symptoms that persist over time.
Trauma and the stress it creates have long been linked to various kinds of pelvic pain, O’Neill noted. Just like chronic lower back pain, acid reflux or night-time teeth grinding are understood to be responses to stress, ongoing pelvic discomfort without an obvious source is likely the result.
“Women carry tension in their pelvis,” according to O’Neill. If heavy, painful periods occur regularly or if pelvic pain arises suddenly and unexpectedly, that indicates something could be amiss.
O’Neill said one major barrier to diagnosis and treatment is an insufficient understanding of the relationship between pain and trauma and pelvic pain — including during and after sexual intercourse — being not normal, with many service members seeking care at military medical facilities such as hers for longstanding issues that date back even before entering service. Military service members tend to report more adverse childhood experiences than civilians do – especially female troops who tend to report these childhood traumas more than their male counterparts.
Women also experience what O’Neill calls a “pain gap”, wherein they’re less likely to receive treatment for both acute and chronic pain than men are. While military medical systems still lag in providing sufficient and flexible care for servicewomen and service members AFAB, O’Neill pointed out that serving in the military may provide access to regular healthcare for some women for the first time ever.
Not all pelvic and uterine conditions are the same, according to O’Neill. Amenorrhea, or the absence of normal periods, may be caused by excessive exercise – this risk increases for service members during military physical training or when underweight or overweight individuals exercise excessively compared with norm. By contrast, menorrhagia – heavy menstrual bleeding lasting more than seven days – is usually trauma-informed according to O’Neill; most cases of menorrhagia can be linked with hormone imbalances which can be managed using birth control pills but O’Neill noted that menorrhagia can also indicate stress-induced disruption of menstrual cycle regulation a potential.
Uterine fibroids, noncancerous growths in the uterus, typically do not require treatment unless they cause symptoms such as pain or heavy bleeding. Rising hormone levels have been linked to their formation.
Link between Sexual Trauma and Chronic Pain
Pelvic pain can be the result of physical and emotional stresses; however, it has also been associated with military sexual trauma (MST). According to data provided by Veterans Affairs (VA), veterans who have experienced MST, combat trauma or post-traumatic stress disorder (PTSD) are up to three times more likely than veterans without these experiences to live with chronic pelvic pain than veterans without such experiences. According to data provided by VA, 1 in 3 female veterans report having experienced MST which increases their risk for developing PTSD as well as stress response symptoms associated with stress response syndrome symptoms like anxiety.
Recognize the signs: Anxiety, agitation or jumpiness could indicate symptoms of posttraumatic stress disorder (PTSD). Tendencies to minimize symptoms could also point towards this disorder as would unwilliness to commit to ongoing medical care – this includes canceling appointments – as well as extreme quietness or withdrawal during appointments.
Crying Without A Clear Cause
Even when MST involves physical trauma, O’Neill said appropriate treatments for survivors such as speaking to medical providers who believe them and validate their experiences can lower the chance of them experiencing chronic physical pain due to MST. She has found that women suffering PTSD symptoms are more likely to experience chronic pelvic pain; evidence of the intimate link between psychological stress and physical symptoms.
Medical providers must listen and believe women who report sexual assault. Provide an opportunity for them to deal with trauma in a safe setting rather than pressuring them into suppressing it further, which only compounding its severity. Ideally, referral should also be made for mental health services as part of any treatment plan.
Military sexual trauma becomes a huge problem when reported but not acknowledged or taken care of,” explained Hauman.
Katie offered similar advice when it comes to pelvic pain in service members of AFAB: seek medical advice immediately and don’t stop until you find the care solutions needed.